Dr. letter regarding surgery part one:
Although longer and more confusing, this letter is far more entertaining. Especially the end. What's even funnier is that my Dad and I were sitting there as he dictated this overly eloquent and verbose letter. And I have trimmed it down pretty considerably.
---
Dear Dr.McMahon:
As a follow-up of today's introductory evaluation of Ms.Hyatt, I write this letter. The patient is being seen for a possible right upper extremity thoracic outlet syndrome. I spend most of our time today listening to the patient's complaints.
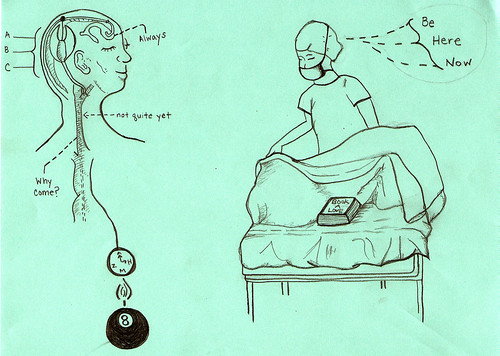
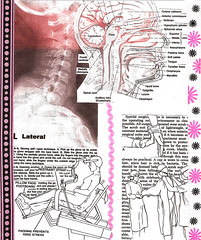
In brief recapitulation, the patient is a twenty-five year old white female with initial swelling of the right hand over a year ago. She underwent subsequent evaluation in Austin, Texas with a subsequent evaluation for persistent symptoms. Chronic adema combined with intermittent pain in the upper arm, forearm, and hand, as she points in the latter to the fourth and fifth digits of the right hand (those which appropriately correspond to the ulnar nerve). She notes as well appreciable pain in the neck. She also has a history of a left iliac vein thrombosis, which was rather extensive secondary to May-Turner's syndrome with an angiolysis in 2001 and subsequent stent placement but not further problems. The patient has been ongoing with physical therapy for the last seven weeks with some appreciable benefit.
The patient remains on significant medication, including Neurontin 300 mg b.i.d., cyclobenzaprine q.h.s., and additional medications she does not recall.
At this point, the patient is noted to have bounding pulses and bilateral radial arteries on standing at military posture, Adson position remains unaffected. Yet, with hyperabduction of the left and right upper extremities, there is adiminution of pulses.
I think most importantly, at this point, the patient is out of school on the basis of pain with any movement of her right hand and arm, as she is right handed. Her function is minimal without great consequence.
At this juncture, the patient has recently and locally seen Dr.Ivica Ducic, whom I know and admire. I was not aware that Dr.Ducic had any interest or expertise in thoracic outlet syndrome, but I do know him to be an excellent individual and surgeon. I know that the patient will be seeing dr. Blair Marshall, who is another outstanding individual. Dr.Marshall is a thoracic surgeon, having finished her training at the University of Pennsylvania and is well known locally, having come through the general surgery program at Georgetown University Hospital and having rotated at Inova Fairfax Hospital.
I have stated that many surgeons have many different opinions about TOS. My own opinion, in regard to Ms. Hyatt's history, I would probably say that I favor some element of TOS in her history; however, at this juncture, I do not see anything that would push me to recommend surgery. Physical therapy, which probably restores individuals to a reasonable function in 50% of the cases, is my recommendation. If, however, the physical therapy does not deem successful, surgical intervention may be necessary.
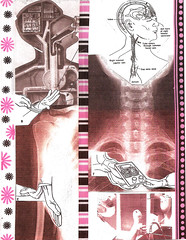
I have further stated to Ms.Hyatt and her father who is accompanying her today that there are numerous, different opinions about thoracic surgery, even if surgery is recommended. I am en enthusiast for a rather traditional first rib resection through a transaxillary approach, taking down all of the attachments tha might effect the ipsilateral subclavian vein, artery, and/or brachial plexus. Other individuals favor a supraclavicular approach with release of nerve entrapment and scalenus anticus division, etc.
My recommendation is that if the patient were to have surgery, she should have one definitive surgery, minimizing the chance for complications or repeat operation where most of the problems come to fruition. On that basis, I recommend the patient defer surgery until it absolutely needs to be performed. This is not to put her in a position of severe end-stage nerve-related symptomatology, but rather until a point where she has proven that she does not benefit adequately with physical therapy, and that she must do something, even if surgery is felt to be a diagnostic maneuver.
I apologize for waxing too eloquent and being verbose. Again, I have stated that there are numerous individuals who think in wildly conflicting ways with regard to this entity, and it is well known to be most often treated in Denver and Dallas where two surgeons in those same communities are very aggressively minded. However, at the same time, it must be kept in mind, at least over the past decade, that thoracic outlet syndrome ........
Finally, Dr.McMahon, at some point......
Again I apologize for this lengthy note, and I ask Dr.Marshall to send me a copy of her evaluation of this patient.
Thank you for allowing me to participate in the evaluation and care of Ms.Hyatt.
Sincerely,
Paul D. Keirnan, M.D.
---
Dr. letter regarding surgery part two:
This is the surgeon who ended up operating on me, as he predicts in the letter.
Dear Scott:
I had the pleasure of seeing Mrs.Hyatt who is currently 25, and, for the past year, has been experiencing symptoms related to Thoracic Outlet Syndrome in her right upper extremity, primarily related to pain, pins and needles, and also coldness/loss of pulse with arm elevation/abduction. She is having most of the symptoms corresponding to the ulnar nerve.
On physical examination, she did have a positive Tinel's sign and tenderness of right but not left brachial plexus. She did have a visually loss of pulse (right hand becoming pale with arm elevation).
Based on her presentations and current findings after a lengthy and detailed discussion, I would summarize my conversation with her as following: I instructed her to obtain a consultation with Dr. Blair Marshall in thoracic surgery for her to discuss whether the 1st rib would need to be addressed at the same time, and I would be planning to perform a brachial plexus neurolysis and anterior scalene muscle removal.
I explained to her that, based on her discussion with Dr. Marshall, the 1st rib can be removed at the same time when the decompression of the brachial plexus and anterior scalenectomy would be performed.
As far as the part of the surgery that I will perform, that would be done through a suprasubclavicular approach with the limited incision that I am using. The possible risks and limitations have been discussed with the patient. Considering that she is currently undergoing physical therapy and is planning to do it through the end of June, then that would be approximately three months of the therapy. Should her symptoms go away by that time, certainly surgery would not be necessary, but based on how abrupt the loss of her pulse is with her current problems with tingling are, I suspect most likely physically therapy might not address her problem and she will require surgery.
In the meantime, thank you again for involving me in the care of this kind patient.
With warm wishes.
Sincerely,
Ivica Ducic, M.D., Ph.D.